May is Mental Health Month and a good time to revisit some of the common myths about smoking and behavioral health.
May is Mental Health Month and a good time to revisit some of the common myths about smoking and behavioral health.
People with behavioral health conditions (mental illness and substance use disorders) smoke at higher rates than those without behavioral health conditions. Alarmingly, people with mental illness and substance used disorders are dying up to 25 years earlier than the general population. The major causes of death are often smoking related cancer, heart disease, and lung disease.1,2
Unfortunately, there are still misconceptions that smokers with behavioral health conditions are not interested in smoking cessation and lack the ability to quit. There are also concerns that these smokers will experience increased psychiatric symptoms when they quit.3 As a result, providers may not include smoking cessation in their treatment plans. Instead, they focus primarily on behavioral health symptom management.
The reality is that people with mental illness and substance use disorders want to quit smoking and can quit successfully. Health care professionals can play an essential role in this process. Providers can bolster a broad health and wellness philosophy for patients by seeing tobacco cessation as a key component of behavioral health treatment and recovery.
Myths and Facts About Smokers with Behavioral Health Conditions
Here are some common myths and facts about smokers with behavioral health conditions.
Myth #1: Persons with mental illness and substance use disorders don’t want to quit.
Fact: The majority of persons with mental illness and substance use disorders want to quit smoking and want information on cessation services and resources.
Several research studies indicate that the majority of persons with behavioral health conditions want to quit smoking and want information on cessation services and resources. 4, 5, 6
Myth #2: Persons with mental illness and substance use disorders can’t quit smoking.
Fact: Persons with mental illness and substance use disorders can successfully quit using tobacco.
There is a growing body of literature indicating that this clientele can quit. For example, results from a large, internationally run randomized controlled trial showed that smokers with behavioral health conditions can quit successfully using nicotine patches, Zyban, or Chantix, compared to placebo, with no significant increase in neuropsychiatric adverse events.7
Myth #3: Smoking cessation worsens psychiatric symptoms.
Fact: Smoking cessation can improve psychiatric symptoms.
This myth has historical ties to the tobacco industry, which directly funded, or monitored, research supporting the idea that individuals with behavioral health conditions (schizophrenia in particular) were less susceptible to the harms of tobacco and that they needed tobacco as self-medication. Fortunately, research has been emerging to debunk this myth.8,9
Myth #4: Smoking cessation will threaten recovery for persons with substance use disorders.
Fact: Smoking cessation can enhance long-term recovery for persons with substance use disorders.10
Research has shown that smoking cessation can encourage and support recovery. For example, a systematic review of 17 studies found that concurrent tobacco cessation treatment with individuals in addictions treatment was associated with 25% increased abstinence from alcohol and illicit drugs six months or longer after treatment. 6
Increasingly, these myths about smoking and behavioral health are giving way to the facts. This is important for a clientele who will benefit greatly from an integrated treatment approach that includes smoking cessation as a priority focus.
For More Information
For more information about smoking and behavioral health, please visit our website or explore our free CE Courses on a variety of smoking and behavioral health issues.
1 Colton, C. W. & Manderscheid, R. W. (2006). Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Preventing Chronic Disease, 3(2).
2 Walker, E. R., McGee, R. E., & Druss, B. G. (2015). Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA psychiatry, 72(4), 334-341.
3 Prochaska, J. J. (2010). Failure to treat tobacco use in mental health and addiction treatment settings: A form of harm reduction? Drug and Alcohol Dependence, 110(3), 177- 182.
4 Prochaska, J. J., Rossi, J. S., Redding, C. A., Rosen, A. B., Tsoh, J. Y., Humfleet, G. L., . . . Hall, S. M. (2004). Depressed smokers and stage of change: Implications for treatment interventions. Drug and Alcohol Dependence, 76(2), 143-151. doi:DOI: 10.1016/j.drugalcdep.2004.04.017
5 Prochaska, J. J.,Reyes, R.S., Schroeder, S.A., Daniels, A. S., Doederlein, A., & Bergeson, B. (2011). An online survey of tobacco use, intentions to quit, and cessation strateies among people living with bipolar disorder. Bipolar Disorders, 13(5-6), 466-473. doi:10.1111/j.1399-5618.2011.00944.x
6 Joseph, A. M., Willenbring, M. L., & Nugent, S. M. (2004). A randomized trial of concurrent versus delayed smoking intervention for patients in alcohol dependence treatment. Journal of Studies on Alcohol, 65(6), 681-691
7 Anthenelli, R. M., Benowitz, N. L., West, R., St Aubin, L., McRae, T., Lawrence, D., ... & Evins, A. E. (2016). Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): a double-blind, randomised, placebo-controlled clinical trial. The Lancet, 387(10037), 2507-2520.
8 Prochaska, J. J., Hall, S. M., Tsoh, J. Y., Eisendrath, S., Rossi, J. S., Redding, C. A., . . . Gorecki, J. A. (2008). Treating tobacco dependence in clinically depressed smokers: Effect of smoking cessation on mental health functioning. American Journal of Public Health, 98(3), 446-448. doi:10.2105/AJPH.2006.101147
9 Evins, A., Cather, C., Deckersbach, T., Freudenreich, O., Culhane, M., Olm-Shipman, C., . . . Rigotti, N. (2005). A double-blind placebo-controlled trial of bupropion sustained-release for smoking cessation in schizophrenia. Journal of Clinical Psychopharmacology, 25(3), 218-225. doi:10.1097/01.jcp.0000162802.54076.18
10 Prochaska, J. J., Delucchi, K., & Hall, S. M. (2004). A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of Consulting and Clinical Psychology, 72(6), 1144-1156. doi:10.1037/0022-006X.72.6.1144
.png?width=278&name=Boost%20your%20immunity.%20(2).png)







 May is
May is 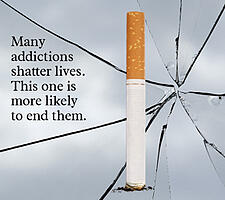 People with mental illness and substance use disorders want to quit smoking and can quit successfully. And mental health professionals can help.
People with mental illness and substance use disorders want to quit smoking and can quit successfully. And mental health professionals can help. 
 People with mental illness and substance use disorders want to quit smoking and can quit successfully. And mental health professionals can help. Until a few years ago, it was uncommon for people with mental illness or substance use disorders to be treated for their tobacco dependence, even though their smoking rates are 2-4 times higher than in the general population.
People with mental illness and substance use disorders want to quit smoking and can quit successfully. And mental health professionals can help. Until a few years ago, it was uncommon for people with mental illness or substance use disorders to be treated for their tobacco dependence, even though their smoking rates are 2-4 times higher than in the general population.